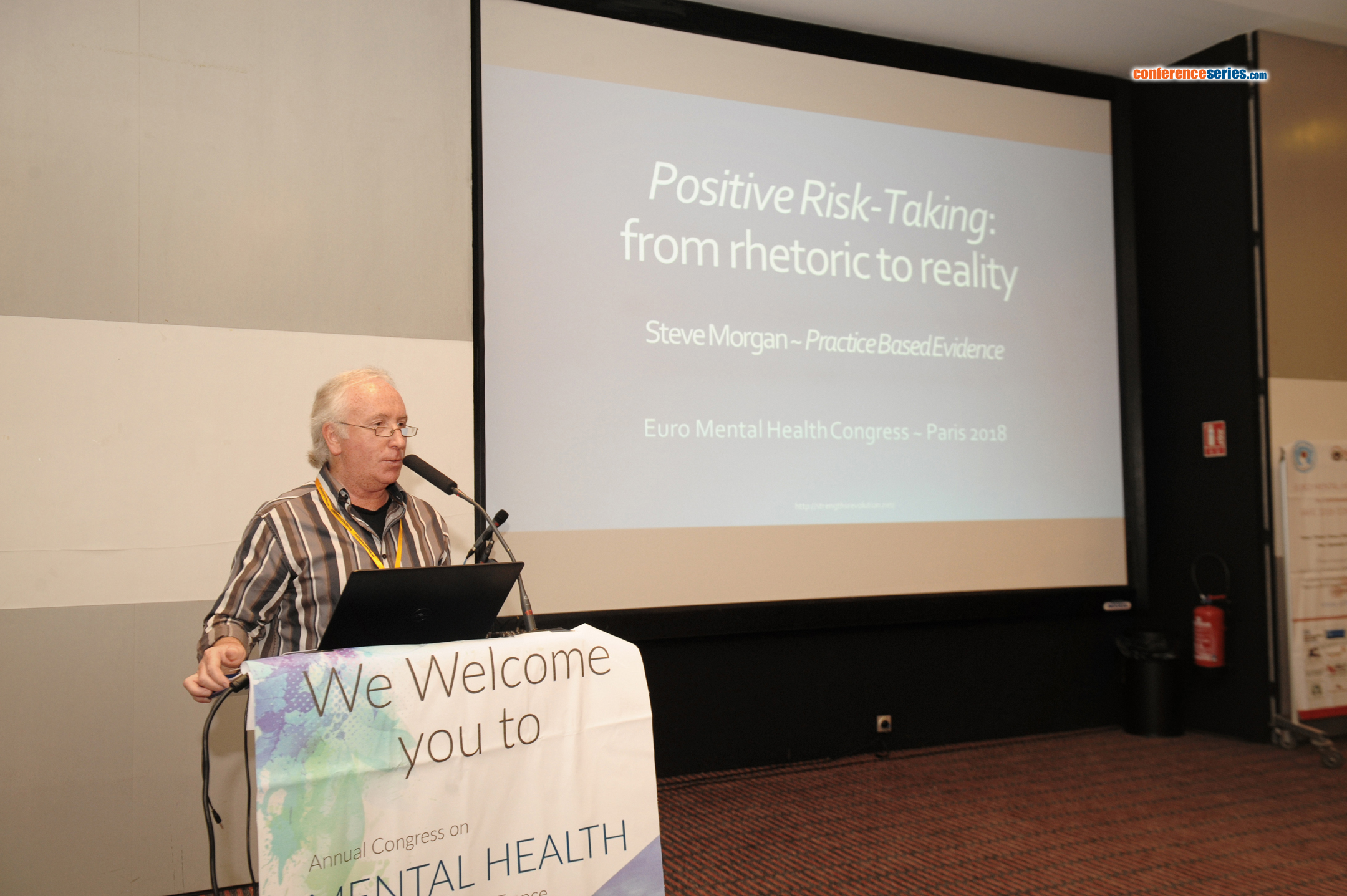
The following was the abstract I submitted for the keynote presentation at the recent Mental Health Congress in Paris (9-11/7/18):
Positive Risk-Taking: From Rhetoric to Reality
Do we pay enough attention to the impact that the language we use has on the people we serve, and the ways in which we serve them? Our adherence to professional jargon more often serves to exclude and/or confuse other people. This is most notable in the language of risk, particularly where the negative connotations can often drive a blame culture and promote an unnecessary risk averse approach. Where is the person within such a picture?
Assessing and manging risk is an essential skill; but, so to is calculated and reasoned risk-taking. My concept of ‘Positive Risk-Taking’, initiated in 1994, brings the language of risk, strengths and person-centred outcomes together in a clear and sharp focus. As a concept, it is underpinned by the principles and practice of good risk assessment and management, applicable to all facets of mental health, wider health, and social care considerations.
The concept is focused on the outcomes, rather than solely being led by the risks. Taking risks for positive outcomesrequires a clear definition and description; but, it is also underpinned by the fully recognized components of mental health good practice… focused and contextualized risk assessment is counter-balanced by a full strengths assessment; supervision and support is complemented by teamwork and team-focused training. Collective decision-making enables balanced and reasoned risk-taking decisions to be made with confidence, and the identification of individual responsibilities for action to be outlined within a thoughtful plan.
Welcoming the audience to the presentation:
A partial link to what you missed!
https://drive.google.com/open?id=1Nmes1fRYvhkBTSLw0rXk8w7yuoxKdTkN
Fielding a question or two:
https://drive.google.com/open?id=1pytmlqXLHoxJc8KKu20wZOT49xjpaKoa
And sharing in the post presentation accolades (holiday snapshots time !!):

 Sunday, March 3, 2019 at 2:59PM
Sunday, March 3, 2019 at 2:59PM